Ghana, Kenya and ten other African countries are first to receive the first ever Malaria vaccine
Due to the overwhelming demand for the first-ever malaria vaccine, 12 African nations will share a total of 18 million doses of RTS,S/AS01 for the years 2023–2025. As part of the Malaria Vaccine Implementation Programme, Ghana, Kenya, and Malawi will receive doses to continue vaccinations in pilot areas.
Over the next two years, 12 countries in various parts of Africa will each receive 18 million doses of the first-ever malaria vaccine. The roll out represents a crucial advancement in the battle against one of the continent’s top causes of death.
The doses that are most needed, where the risk of malaria disease and mortality among children is greatest, are given priority in the Framework for Allocating Limited Malaria Vaccine Supply, which has been applied to decide the allocations.
The Malaria Vaccine Implementation Programme (MVIP), coordinated by WHO and supported by Gavi, the Vaccine Alliance, the Global Fund to Fight AIDS, Tuberculosis and Malaria, and Unitaid, has been providing the malaria vaccine to Ghana, Kenya, and Malawi since 2019. Since its administration to more than 1.7 million kids in Ghana, Kenya, and Malawi in 2019, the RTS,S/AS01 vaccine has been proven to be both safe and efficacious, leading to a significant decline in both severe malaria and child mortality. The malaria vaccine has attracted interest from at least 28 African nations.
Nine additional nations, including Benin, Burkina Faso, Burundi, Cameroon, the Democratic Republic of the Congo, Liberia, Niger, Sierra Leone, and Uganda, will be able to incorporate the vaccine into their routine immunisation programmes for the first time thanks to the initial 18 million dose allocation, in addition to Ghana, Kenya, and Malawi. This distribution round takes use of the vaccination doses that Gavi, vaccination Alliance has access to through UNICEF. The first doses of the vaccine should arrive in countries in the final quarter of 2023, and they should begin to be distributed by early 2024.
When widely used in conjunction with other interventions, this vaccine has the potential to have a significant impact on the fight against malaria and can avert tens of thousands of additional deaths each year, according to Thabani Maphosa, managing director of country programmes delivery at Gavi, the Vaccine Alliance. As we expand to a new total of 12 nations, we must ensure that the doses we already have are utilised as efficiently as possible while working with manufacturers to help ramp up supply. To do this, we must apply all the lessons we’ve learned from our pilot projects.
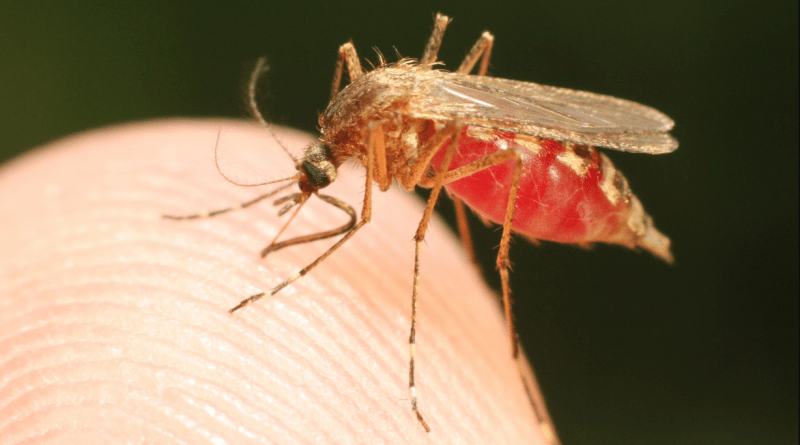
Nearly 500,000 children under the age of five continue to die each year from malaria, which continues to be one of Africa’s deadliest diseases. In 2021, malaria will be responsible for 95% of cases and 96% of fatalities worldwide.
According to UNICEF Associate Director of Immunisation Ephrem T. Lemango, a kid under the age of five dies from malaria almost every minute. “These deaths have long been preventable and treated, but the introduction of this vaccination will increase the chances of survival for children, particularly those in Africa. We hope that as supply grows, many more kids will gain from this life-saving development.
Families and communities rightfully desire to provide their children with the malaria vaccination since it has improved child health and child survival. According to Dr. Kate O’Brien, WHO Director of Immunisation, Vaccines and Biologicals, this first distribution of malaria vaccine doses is prioritised for children who are most at risk of dying from malaria. “The strong reach of childhood vaccination and the high demand for the vaccine will promote access equity for malaria prevention and help save many young lives. Till all at-risk children have access, we will put forth unwavering effort to improve supply.
Given the limited supply in the early years of the roll-out of this new vaccine, WHO gathered expert advisors in 2022, primarily from Africa, where the burden of malaria is greatest, to support the creation of a Framework for the Allocation of Limited Malaria Vaccine Supply. This Framework would serve as a guide for where initial limited doses would be allocated. The Framework suggests that vaccine distribution start in the places with the highest need and is founded on ethical values and a foundation of solidarity.
Representatives from the Africa Centres for Disease Control and Prevention (Africa CDC), UNICEF, WHO, and the Gavi Secretariat, as well as members of civil society and independent consultants, participated in the Framework implementation group that put the framework’s ideas into practise. The Senior Leadership Endorsement Group of Gavi, WHO, and UNICEF evaluated the suggestions and approved them.
By 2026 alone, the demand for malaria vaccines is projected to reach 40–60 million doses annually, increasing to 80–100 million doses annually by 2030. In addition to the RTS,S/AS01 vaccine, developed and manufactured by GSK and subsequently supplied by Bharat Biotech, it is anticipated that the WHO would shortly prequalify the R21/Matrix-M vaccine, created by Oxford University and manufactured by Serum Institute of India (SII). Gavi just revealed its plan to promote raising supply to accommodate rising demand.